
BY: MELINDA EVANS
Ask any dietitian, and they’ll probably tell you that their clients are asking them about the ketogenic diet more than any other recent ‘fad’ diet. Popular headlines have proclaimed it the miracle diet to shed weight, boost energy, reverse diabetes and send cancer into remission.
But does this diet live up to its hype? What could it possibly have to do with recovery from traumatic brain injury (TBI)? And more importantly, is it safe?
The Ketogenic Diet
The ketogenic diet started out as anything but a fad. It was developed almost 100 years ago to treat children with epilepsy that didn’t respond to anti-epileptic medications. By definition, it is a very low carbohydrate (less than five per cent of total energy per day), high fat (about 80 per cent of energy) and moderate protein (15 – 20 per cent) diet.
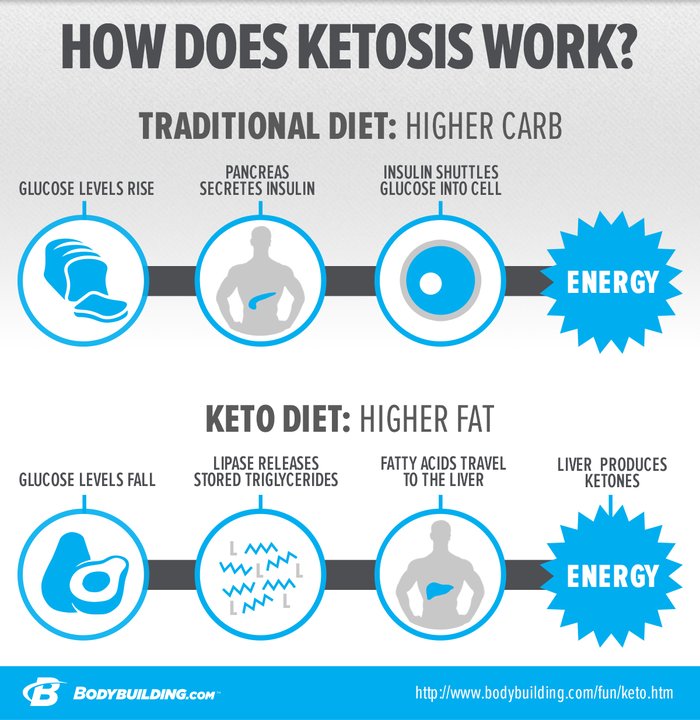
This is vastly different from Health Canada’s recommended macronutrient distribution, which is 45 – 65 per cent carbohydrate, 10 – 35 per cent protein and 20 – 35 per cent fat. Since glucose (a carbohydrate) is our body’s preferred source of fuel, this high fat / low carbohydrate diet essentially tricks the body into believing it is in a state of starvation. The liver begins to convert fat into ketones (hence the name), and the brain’s cells are forced to adapt. The result, for someone with intractable epilepsy, can be a 50 to 90 per cent decline in seizures.
Once medical practitioners observed the effectiveness of ketosis for the treatment of epileptic seizures, they started to wonder whether it might help other neurological injuries and neurodegenerative disorders, including hypoxia, ischemic stroke, ALS, Alzheimer’s disease, Parkinson’s disease, and of course, Traumatic Brain Injury.
Benefits of Ketosis for Traumatic Brain Injury
For a multitude of ethical and practical reasons, it is next to impossible to perform randomized clinical trials on humans with TBIs, so the research we have that looks at the role of the ketogenic diet has been done in animals. The findings are promising though, and suggest that following injury, when the brain’s need for energy is high but its ability to metabolize glucose is impaired, ketones might provide an alternative and efficient source of energy.
Following trauma, brain cells are at increased risk of oxidation, cell death and DNA damage, and the presence of ketones and absence of glucose may reduce oxygen available for oxidation and guard cells against free radicals and DNA damage, while increasing cerebral blood flow.
Knowledge Gaps
This is an exciting prospect, but we still need a lot of answers before we can incorporate it into practice. We don’t know which type or severity of brain injury might respond well to ketosis, or whether it is best achieved through fasting, the ketogenic diet or even intravenous provision of ketones. It is unclear whether ketosis is helpful only initially after injury, or if it will support brain recovery if used for a longer period of time. It’s possible that a modified and less restrictive form of the ketogenic diet would work just as well as the standard diet, and some studies suggest that it might be even more effective when supplemented with certain nutrients, including medium chain triglycerides and branched chain amino acids.
Challenges of the Ketogenic Diet
There are several challenges with the ketogenic diet, the first being compliance. Since it is extremely restrictive, it is difficult for most people to stick to the diet long-term. It excludes entire food groups (grains, fruits and many vegetables), increasing the risk of nutrient deficiencies including sodium, potassium, chloride, vitamin D, calcium, magnesium, selenium and zinc. Among other issues, these deficiencies can impair bone healing and increase the risk of osteopenia and bone fractures. For people with pre-existing kidney disease or renal failure associated with trauma, the high protein intake that usually accompanies a high fat diet may not be appropriate. And of course, with a high fat diet there is concern about elevated cholesterol levels. Studies evaluating the use of the ketogenic diet in children found elevated triglyceride, and total, HDL and LDL cholesterol levels at 6 months and 10 years, making this diet risky for people predisposed to coronary artery disease. Long-term use has also been associated with growth retardation in children, low-grade acidosis, constipation, dehydration, vomiting and nausea.
The Future of Ketosis in Brain Recovery
So, is the ketogenic diet the future for TBI treatment? Will it minimize brain injury and help to rehabilitate cognitive function, memory and recall? Maybe. We don’t have enough information yet to make it standard practice, and it certainly should never be implemented without careful monitoring from a physician and dietitian.
More research in humans is needed before we can give a final verdict, but what we know so far about ketosis and the brain is promising!
FEATURED IMAGE: Photo of a Cauliflower Crusted Grill Cheese Sandwich via KirbieCravings.com
Melinda Edmonds is a Registered Dietitian with Aimee Hayes & Associates. She is a registered member in good standing with the College of Dietitians of Ontario and an active member of Dietitians of Canada. The focus of her practice is on the application of evidence-based nutrition therapies to optimize clients’ health, nutritional status and well-being in order to augment their quality of life and rehabilitation outcomes.
Aimee Hayes and Associates provides nutrition rehabilitation services to individuals with acquired and traumatic brain, spinal cord, and orthopedic injuries. Our diverse and dynamic team of Registered Dietitians works collaboratively with clients, families, caregivers and interdisciplinary rehabilitation teams to optimize nutrition in order to promote our clients’ wellness and recovery.
Filed under: Health and ABI, Uncategorized Tagged: Ketogenic Diet
![]()




